Pain is often experienced as a fatality. Omnipresent in consultations, it is said to be the cause of ⅔ of medical visits. Although it is difficult to quantify and qualify, research is refining its findings on these aches that so disrupt our daily lives. Chronic pain covers a wide range of symptoms and affects a growing number of patients. How can they be managed? Coping with chronic pain means understanding its issues and its different forms, which is what we will uncover in this article.
Understanding chronic pain for better relief
What actually happens when you are in pain?
The International Association for the Study of Pain (IASP) explains that “pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, described in these terms”.
Pain appears to be subjective, closely linked to the patient’s feelings, which makes its study, and therefore its detection, more complex. Nevertheless, the painful information follows a defined pathway in the body. For example, in the case of a burn, the nerve endings in question will be stimulated. These may be associated with muscles, joints, viscera or skin. This data travels along the nociceptor nerves, to the spinal cord and finally to the brain. The signal is only interpreted at this last stage, when the brain deciphers it as painful. The limb in contact with the burning surface will have been withdrawn through the reflex arc of the spinal cord.
Acute pain acts as an alarm to protect the body from a thermal, chemical or mechanical stimulus. However, when pain becomes chronic, this mechanism is no longer justified, and the pain becomes a disease in itself.
The WHO definition of chronic pain
Pain is defined as chronic when it lasts or recurs for more than three months. The chronic pain syndrome appears in the International Classification of Diseases (ICD-11) under two categories: primary and secondary.
Primary chronic pain
Considered a disease in its own, it is characterised by disability or emotional distress that can only be explained by a diagnosis of chronic pain. This category includes :
- chronic widespread pain such as non-specific lower back pain, fibromyalgia or complex regional pain syndrome;
- chronic musculoskeletal pain;
- headaches;
- primary conditions such as irritable bowel syndrome or chronic pelvic pain.
Secondary chronic pain
This time, chronic pain is a symptom of an underlying disease and therefore falls into one of the following six categories:
- chronic cancer-related pain ;
- chronic neuropathic pain;
- chronic post-surgical or post-traumatic pain;
- chronic headache or orofacial pain;
- secondary chronic musculoskeletal pain (as a result of persistent inflammation);
- secondary chronic visceral pain.
What are the types of chronic pain?
Depending on the physiological mechanisms involved, different forms of pain can be identified:
- inflammatory pain, associated with inflammation phenomena, is often joint pain;
- neuropathic pain, linked to disorders of the central and peripheral nervous system, such as damage to the sciatic nerve or the spinal cord;
- mixed pain, which includes both inflammatory and neuropathic aspects, and is generally found in cancer or after surgery.

Overview of the situation
Chronic pain affects a growing number of patients. Its detection and treatment are the subject of intense scientific research. Where do we stand exactly?
How many people are affected by chronic pain?
According to Inserm (French National Institute for Health and Medical Research), 30% of the general population is affected by chronic pain, and this incidence increases with age. Women and disadvantaged socio-professional categories are said to be the most affected, as are manual occupations and people living in rural areas. A worrying factor is that ⅔ of these cases suffer from pain of moderate to severe intensity. On the other hand, chronic pain regularly accompanies depression, sleep disorders and overall anxiety.
Which parts of the body are most often mentioned? The back, neck, shoulders, head and abdomen. The notorious migraine, for example, affects 11 million people.
The state of scientific research on chronic pain
A great deal of work is being done to personalise the treatment of chronic pain, both for existing drugs and those in development. Nevertheless, the search for therapeutic approaches to chronic pain appears necessary to offset the long-term side effects of drug solutions. Acupuncture, sophrology and hypnosis are non-pharmacological approaches that have become very important in pain centres.
The understanding of the mechanisms involved in chronic pain has led to the realisation that pain is not solely neuronal. Subsidiary cells of the central nervous system and some immune cells are also involved in its occurrence. Furthermore, the discovery of the phenomenon of peripheral and central sensitisation has highlighted the hypersensitivity to pain that exists after a surgical operation or a nerve lesion. This latter finding explains why, in some patients, subsequent painful events are experienced in an exacerbated manner.
On the other hand, pain can now be identified, visualised and even quantified at the brain level using brain imaging techniques such as functional MRI (fMRI). In France, the Inserm Pain Research Network brings together teams working on this topic and contributes to advances in the management of chronic pain.
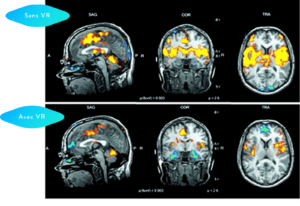
Group analysis by fMRI showing no VR for 3.5 minutes versus VR for 3.5 minutes.
Subjects showed a significant reduction in pain-related brain activity when in virtual reality: anterior cingulate cortex, primary and secondary somatosensory areas, insula and thalamus.
The contribution of virtual reality for coping with chronic pain
Amongst cognitive-behavioural therapies (CBT), EMDR (eye movement desensitisation and reprocessing) and hypnosis, virtual reality appears to be a significant player in coping with chronic pain. It is a non-medicinal, non-invasive solution with real therapeutic potential. Its effectiveness has already been proven for the treatment of acute pain and pre-operative care. Its use in chronic pain is therefore particularly relevant.
A scientific study on the effect of virtual reality in chronic pain values its analgesic action during and after the session. Although further experiments are needed, these initial findings highlight this solution to manage chronic pain.
Virtual reality can modify neurosensory perceptions of painful areas. In other words, it focuses the brain’s attention on an activity rather than on the pain. The realistic 3D environments are not the only asset of this non-pharmacological treatment. Indeed, the principles of hypnosis, music therapy and cardiac coherence are used in synergy to relieve patients’ anxiety and provide well-being.
Scientific research is very active and has led to a better understanding of chronic pain syndrome and improved patient care. Therapeutic techniques have a major interest in these treatments and virtual reality appears to be an effective solution for coping with chronic pain. We have no doubt that our virtual reality headsets bring relief to the pain experienced and we suggest that you try them out to make your own opinion. Do not hesitate to contact us to arrange a demonstration.